
When you got diagnosed with PCOS, the first question for you wasn’t about the treatment options that are available out there (or maybe it was, was maybe you don’t have the diagnosis and are just exploring!).
But if you have PCOS, one thought that keeps playing on your head is probably, why me? Why did I get PCOS? And then there comes what can I do?
And if you don’t have PCOS, you are probably worried that you might have it, when your period delays by days/weeks or when acne breakouts or your cramps feel as is someone stabbed you!
By the end of this blog, you will have found answers to (not all) but at least some of those questions.
Understanding PCOS
PCOS = Polycystic Ovarian Syndrome (Sounds complicated??)

PCOS is somewhat complicated in real life too!
It is not just about one hormone or one organ.
PCOS involves a pattern of interaction between your hormones, metabolism, and your reproductive system (but is not limited to it).
But, let’s start with something simple!!
What is happening inside your body on PCOS?

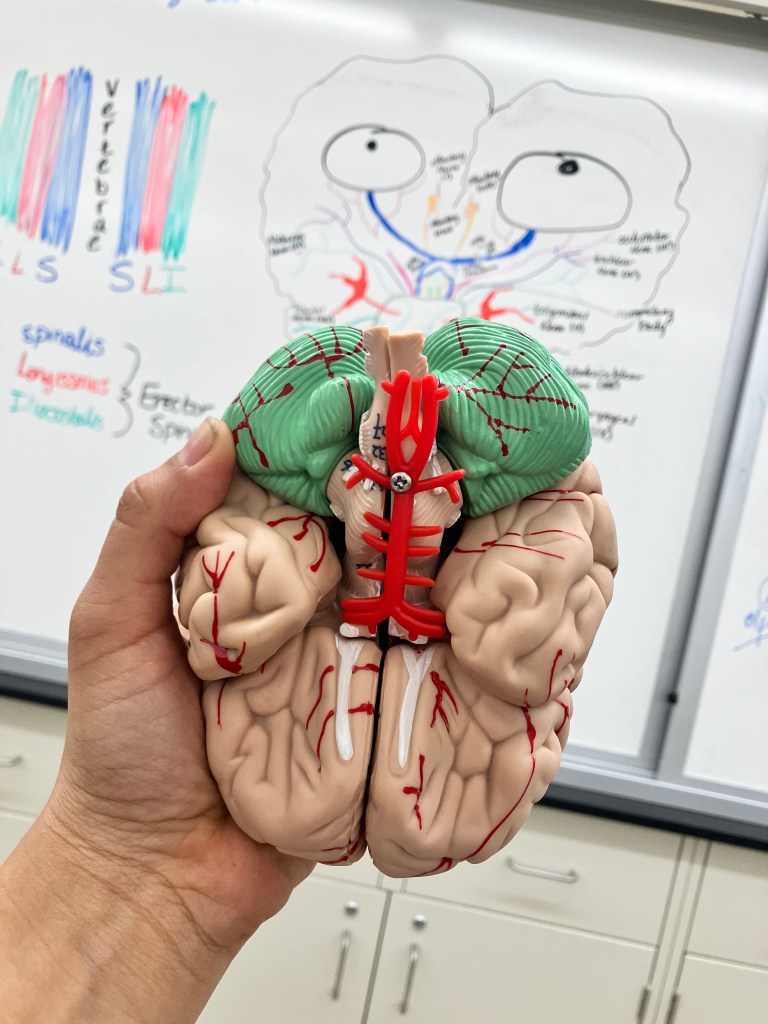
So every month, your ovaries prepare tiny sacs called follicles and each follicle has an immature egg.
Normally, one follicle matures fully, and releases an egg during ovulation, and the rest fade away. This process is guided by hormones interacting between the brain and the ovaries. In PCOS, that process is disrupted.
But it is not that your ovaries have become dysfunctional. Your ovulation is irregular, and this can mess up with your menstrual cycle [delayed period, no period, even early period].
Those unruptured follicles can gather together along with the other follicles, and this can create that multiple cyst (polycyst) image on your ultrasound which is where the Polycystic Ovarian term came!
However with time, scientists noticed that some people had polycystic-appearing ovaries without the classical symptoms (excess hair growth, acne, menstrual abnormalities) while others had clear PCOS symptoms without the polycystic ovarian appearance.
This suggested that the ovaries might be responding to signals rather than malfunctioning on their own.
A major shift came in the 1990s through the work of endocrinologist Dr. Andrea Dunaif, who showed that many people with PCOS had insulin resistance, even when they were not overweight.
Her research revealed that insulin was not just a blood sugar hormone, but one that directly influenced ovarian hormone production.
When insulin levels remain elevated, they can signal the ovaries to produce more androgens, hormones that are normal in all bodies but may be higher in PCOS. Increased androgen activity can interfere with follicle maturation, making ovulation less regular.
Androgen is also known for giving those pimples that you don’t want at all!
This helps to explain why PCOS looks different in different people.

But,
How?
PCOS involves hormonal and metabolic communication. Hormones act as messengers, and tissues act as listeners. In PCOS, the messages may be similar, but different tissues respond more strongly. In some bodies, insulin resistance mainly affects the ovaries or skin, leading to cycle changes or acne. In others, it influences muscles, fat tissue, or energy levels, with fewer visible signs. Androgens also act differently depending on tissue sensitivity, which is shaped by genetics. The ovaries, in this context, are not malfunctioning. They are responding to the metabolic environment they are in. So, having poly-cyst is also a part of PCOS not just the one.
Is PCOS your fault?
So far, we have been talking what is PCOS, but I know you are still eager to know why does it happen.
Is it your hormones? Is it your diet? Is it genetics?
The answer is yes! And what I mean is, it could be anything, the exact cause is still unknown but it could be due to various reasons as such-
Genetics
PCOS often runs in families. Certain genes can affect insulin signaling, androgen levels, and ovarian function. Genetics don’t guarantee PCOS, but they can make the body more sensitive to hormonal and metabolic stress.
Excess of certain hormones
Hormones like insulin and lutenizing hormones signal the production of androgens. Excess of these hormones can trigger more androgen that can disrupt the ovulation.
Metabolism also plays a role
As mentioned above excess insulin can trigger anovulation (i.e absence of ovulaion). Some of the metabolic disorders like diabetes can cause insulin resistance, which can cause more insulin production.
Yes, girl your Lifestyle plays a role
For any condition that is affected by metabolism and hormones, your lifestyle always plays some role. Although stress, diet, exercise, don’t directly cause PCOS, they can affect the extent of symptoms, the recovery process, and even impact your hormones levels.

So, is it really your fault that you have a PCOS?
Short answer no! Because noone chooses to have a condition that affect their lifestyle significantly.
But here is what we can do : be accountable of your lifestyle choices, be aware of the condition itself, be updated with research being done on PCOS, and support each other!!!
I know you still have one more question – how to heal PCOS?? That will be my next blog!
Signing off for now!!
-Sneha
References (click click)


Leave a comment